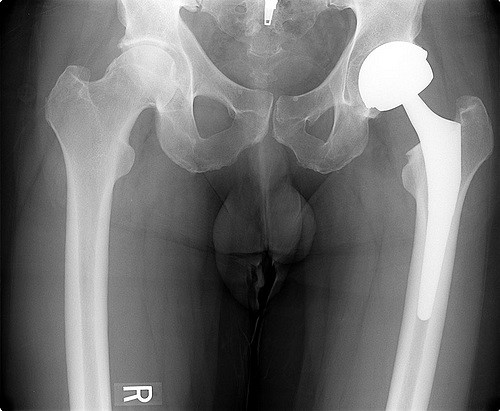
Firstly, this scheme is a direct attack upon the universality of the health system. Those over 75 will receive better access to care than those under 75. With time, if the scheme works perfectly, and is combined with the many other improvements to the health system which are needed, those under 75 may achieve parity, but it is unlikely. The Coalition claimed that it was retaining universality with its changes to Medicare, but what it was talking about was universal access to an inadequate rebate for community doctoring, universal access to a long waiting list at public hospitals, and universal access to higher PBS copayments. The Labor Party’s claim that the Medicare Gold proposal is part of a universal health care system is similarly misleading. Imagine the 73 year old wife will wait two years in pain for a hip replacement, whilst her 75 year old husband has his knee arthroscopy within weeks. As for the much more needy 35 year old unable to work or look after the kids while she waits for her hip surgery from her rheumatoid arthritis, this scheme leaves her with nothing. Statistics indicate that over 75s need more services, but the 35 year old is not a statistic. Statistics also indicate that those on pensions and health care cards need more services. But the proposal to increase the GP Medicare rebate just for those people has been justifiably criticised for eroding the universality principle as it leaves needy non card holders with a different level of access to care.
Secondly, although there is no specification in the proposal as to whether the care is given in a public or private hospital, it would seem very likely that much of the extra care would occur in the private sector (better characterised as the publicly subsidised pseudo private sector). The consequences of the increased demands on the private sector would be a further expansion of the private sector with a further resource drain on the public sector. Thus, doctors, nurses, and other professionals, all of whom are already in short supply in the public sector, would move to the private sector where work conditions are better and there is more work to be done.
Thirdly, despite the comments in the article, the issue of overservicing in a fee-for-service setting remains a major concern. I note the comparison with the Veteran’s Affairs Gold Card system and ask whether the comparison of utilisation rates by Veterans with a Gold Card without a disability is an appropriate comparitor, even when aged standardised. What about those with a disability? Does the male/female ratio make a difference? Does the fact that Gold Card Veterans have better easier access to specialists, allied health, and perhaps GPs, have any impact? There is strong evidence that fee-for-service funding is associated with a much higher level of utilisation of services than non fee-for-service funding.
Despite these criticisms, the proposal at least recognises that access to hospital services is a major concern. This is in stark contrast to the Government’s position, which is that it has no responsibility for hospitals, despite it being responsible for inadequate Aged Care services leading to access block, inadequate primary care leading to avoidable admissions to hospitals, underfunding through the Australian Health Care Agreements, and staff shortages in public hospitals contributed to by its PHI rebate which has expanded the private hospital sector which must result in staff transfers from public to private.
Tim Woodruff is the President of the Doctors Reform Society.