Recent welcome announcements from the federal government about increased funding for the care of people with mental illness have mentioned their intention to explore ways of funding, through Medicare, services other than those provided by a medical practitioner. The report of the Productivity Commission on the health workforce is critical of the tight preserve many health professions exercise over their territory. It acknowledges the value of maintaining clear professions that complement each other and does not advocate the training generalists who have no professional heritage. But with too few people to do the work, it needs to be shared among professions better than at present, and this is especially so in relation to serious and continuing illnesses of which mental illness is preeminent.
For decades publicly-funded aged care in Australia has demonstrated how health professionals of different persuasions — doctors, nurses, occupational therapists and physiotherapists — can work effectively together in teams. But in the private sector, of which general practice is the largest component, collaboration is not so easily achieved unless paid for by the patient and their health fund.

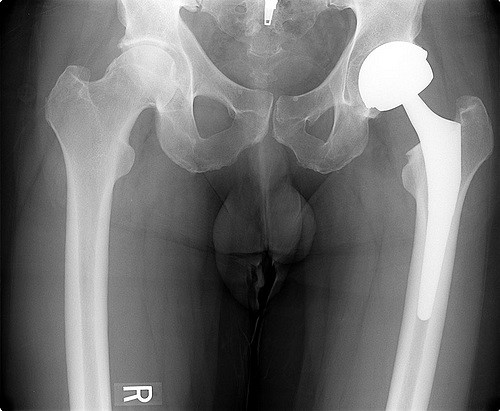
Thanks to Bill Leak. |
But there are encouraging signs of change. Treatment studies in several hundred general practices have shown how mental health care can be shared between professions to good effect. Since 2001 federally-funded treatment trials of collaborative care between general practitioners and primary care psychologists with certified skills have helped patients with common disorders including depression and anxiety. Over 25,000 patients have received publicly-funded treatment with success rates around 90%. Treatment is both short-term – up to six sessions – with six more if needed. The average treatment consists of four visits at a cost of $400.
Helen, a 37 year old teacher and mother of two children, was referred by her general practitioner to the local primary care psychologist for a severe panic disorder. Her first attack came out of the blue at a family party and led to her admission to hospital. She experienced severe palpitations, causing concern about a heart condition, but tests were negative. While on extended sick leave from work, her general practitioner referred her for four sessions of treatment from a clinical psychologist. She gained an understanding of the symptoms of panic and learned to recognize and counteract the signs of stress contributing to her attacks. A long lead-up of cumulative distress and tension, including bereavement and financial pressures, had led to her condition, and this was explored. She was taught techniques to manage stress more effectively, to balance commitments and to set limits on demands. She had planned to quit her job but she returned to work within weeks. She received four treatments over two months and had two follow-up sessions.
The general practitioners involved in the collaborations seem to be generally well satisfied with it and do not see it as stealing their income. At present only a minority of general practitioners can access these services, but this may well expand under the new Medicare provisions. Detailed costing has not been done, and should be.
Beyond concerns with money, the trials also address a health workforce problem. Psychiatrists are a scarce commodity in unrelenting demand. Rural patients find it difficult to access psychiatric services located primarily in urban areas. Clinical psychologists are more widely dispersed and numerous. There are at least 5,000 psychologists in Australia with sufficient clinical expertise to function as mental health specialists and who could provide the style of non-pharmacological interventions that many persons with less severe disorders both need and seek
The extension of Medicare to other health professionals is one that must be welcomed when good care can be provided to people in need, people who may otherwise miss out. In the U.S. and Britain, primary care psychology is established as a mental health specialty in which clinical and health psychologists provide collaborative care with general practitioners and physicians for patients.
The cost of bringing clinical psychologists into Medicare can be estimated by assuming that there are 2000 practitioners available who would bill up to $50,000 each year, at a cost of $100 million. Assuming they charge $100 an hour, and that each patient requires six one-hour sessions, 167,000 additional patients could be treated each year.
The trials of similar services in Australian general practice described here suggest that this model might well be developed across Australia to good effect. Overuse of these services is always possible, and limits on volume of services should be set. This is difficult, but by no means impossible, in a fee-for-service environment, but a healthy respect for the infinite capacity for expansion that characterizes the health system demands such limits before budgets blow out and recrimination follows. For the moment, these trials give hope to patients with other serious and continuing illness such as heart failure that better care can be provided to people in need without the different health professions sharpening their swords and going into battle over turf.
Recommendations:
1. That the research trials of psychologists working with general practitioners be used as the basis for the expansion of Medicare to cover their services in the care of mentally ill patients.
2. That policy be developed to control possible over-servicing as a result of these changes in Medicare.