Health is our largest industry. Australian spending on health has increased significantly in recent years from 8.3% of GDP in 1993/94 to 9.7% of GDP in 2003/4, or $79 b. Compared to the OECD average we have spent at an increasing rate in the last decade. The fastest growth area of spending has been pharmaceuticals. The ageing population and new medical technology have been important factors driving this increase.
We should examine carefully whether we are getting value for money. It is time for Commonwealth and State Treasurers, as well as Health Departments, to examine the factors driving up increased cost and consider areas where reform could achieve lower unit costs. I don’t believe it is necessary to increase spending on health, at least not until we have addressed some of the obvious dysfunction and inefficiency in a system which is coming to the end of its design life. Let me highlight those areas where significant reform would produce better value for money.
Setting priorities in health — making choices
We cannot have all we want in health. Choices have to be made. Health resources and dollars are limited, yet demand continues to increase quite dramatically. That demand is driven by community expectations; providers (particularly those who work on a fee for service basis); pharmaceutical companies and patient groups who regularly urge us to spend more on new wonder drugs, and medical technology companies which are developing quite remarkable but expensive new equipment. Many of these discoveries and breakthroughs, and interventions, are valuable in their own right. But we can’t afford it all. Choices have to be made, not only within the health field, but also across portfolios. Is it better for example to spend $10 m on state-of-the-art equipment in an ICU for road accident victims, or spend $10 m on speed humps on the roads?
Ministers have to make final decisions but an informed community must be engaged for example through citizens’ juries, in helping to advise where limited resources should be spent. I emphasise an ‘informed’ community in which individuals are fully briefed to make informed judgements that enables the individual to contest the view of experts. Invariably the health debate is between ministers and doctors, and the community is excluded. My observation is that when community groups are well informed about priorities and the options involved, they invariably put, for example, mental health and aboriginal health at the top of the list well ahead of hospitals and hospital beds. Informed community members usually give much lower priority to life-extending interventions in the last stage of terminal illness, some fertility treatments and hospital super-specialties. Making choices is hard, but my experience is that when the community is well informed it comes to realistic and what I think are sensible decisions on the priorities of health spending. We must obtain informed advice from the community. Otherwise, the system will be under continual pressure, unrealistic demands are asked of very professional and dedicated staff, and sensible long-term reform will be impossible. Governments will be reacting to the latest crisis, real or media induced. Priorities have to be set. We can’t afford everything.
Hospital versus primary care
We have a very hospital-centric system. Hospitals take well over half of state government health budgets. Hospital expenditure represents about 30% of total health costs. Hospitals are a vital part of the health system, but they should be a last resort. Unfortunately, they are often a first-resort and hospitals are often seen as synonymous with health. The public debate about health is invariably dominated by hospital interests, particularly specialists who manipulate sectional and local interests. The media-savvy dominate the debate, particularly over hospital beds. In the political clamour, the important (mental and aboriginal health) is blotted out by the hospital sector. Hospitals and hospital beds are like the family refrigerator. Whatever the size, it will invariably be full. If I could change the metaphor, it is like cars and roads. As we improve the road system, we bring on more cars. The whole process is quite circular.
At least 30% of persons in hospitals need not be there if there were suitable and invariably cheaper options for health care in the community or the home. Our health system needs to be driven through primary care, particularly around general practice. This is a trend worldwide, but Australia is slow responding. All health systems are under severe strain, but those systems grounded in primary care as in the UK and NZ, are in my view performing better than others, both as regards to costs and services. We need not more hospitals and hospital beds, but community health centres committed to both health maintenance and treatment of illness, and staffed by multi-skilled teams.
Quality and Safety
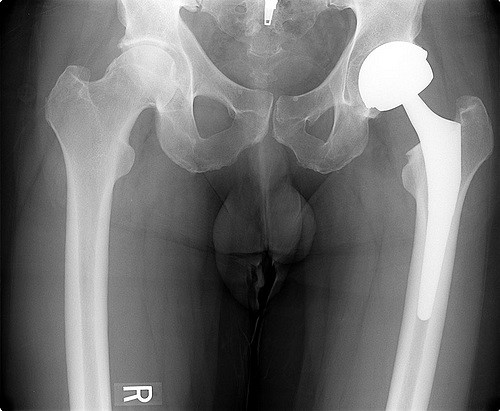
Hospitals are dangerous places for patients. Significant financial costs are also involved in these ‘adverse events’ or mistakes. The national cost of avoidable ‘adverse events’ was conservatively estimated to be over $4 b in 1995/96 (see ‘The Quality in Health Care Studies in 1995′). The financial cost would be much higher today but no reliable figures are available as far as I know. This is a problem both in public and private hospitals. For example, the estimated revision or ‘re-do’ rate for hip and knee replacements in Australia is 20% to 25%. In Sweden, it is 7%. (Source: National joint Replacement Registry). Substantial inconvenience and cost to the patient is incurred in these revisions. There are 65,000 hip and knee replacement procedures in Australia each year. A primary procedure costs about $15,000. A revision procedure costs anywhere between $25,000 and $50,000. Lowering the revision rate to something approaching the Swedish rate would save up to $200 m per annum. The problem is not with individual surgeons, but with obtaining up to date data, assessing new technology and responding quickly when problems are identified. It is an information and systems issue.
Despite numerous enquiries and committees, there are several reasons why we have not responded adequately to quality and safety problems. Unlike the airlines, hospitals have been inclined to play the blame game and pillory individuals who make mistakes, which in turn encourages cover-up. The airlines have been successful in safety because they have developed a transparent safety culture which addresses system failures which are invariably the cause of accidents. Another reason for the poor quality and safety record in health is that hospitals, particularly in country areas, and some specialties within hospitals, are maintained for political reasons when there are not enough experienced staff available. Another important cause of the poor quality and safety record is the lack of integration of corporate governance and clinical governance. They often work independently of each other. In every organization, particularly large companies, there is a disconnect between the top of the hierarchy where visions and strategies are set, and the delivery of services lower down in the organization. It is a very serious problem in hospitals. The decisions made by clinicians in hospitals dramatically affect lives and costs yet they are often disconnected from the corporate governance of the whole organization. It is often not at all clear who is in charge and who is responsible. The CEO often gets the blame for clinical outcomes over which he or she has little or no control, as we saw in Bundaberg. There is quite confused governance in hospitals. I am not really sure who runs them.
The Commonwealth has provided hundreds of millions of dollars to subsidise medical insurance premiums for doctors. This is addressing the symptom and not the problem. The real solution involves accreditation, particularly of small hospitals, reliable and efficient records, better hospital systems, consolidation of specialist services, clinical accreditation, peer review and importantly, integrated and effective governance. But probably above all else, what is necessary is the need for openness and transparency. So many quality and safety issues are hidden for fear of professional, legal, financial or political repercussions. A veil of silence invariably descends. A scapegoat is found. But the system goes on as before.
Commonwealth State relations
The issue of blame and cost shifting is of growing public concern. I have seen estimates of the cost of fragmentation between Commonwealth and State programs ranging from $1b to $20 b per annum. I think it is much nearer the former figure.
There are major health dividends in the solution to this Commonwealth and State fragmentation. The community would welcome change. I don’t think the community is particularly concerned who delivers the service, provided it is delivered well. It seems to me important that the Commonwealth set national policies and standards and that as far as possible, services are delivered at the most local level possible. The principle of subsidiarity means that a function should be carried out at the lowest level of government able to exercise it effectively. It is important particularly in a country as large and diverse as Australia.
A Commonwealth takeover of State health functions in unrealistic, as is the reverse. I think it is also unlikely that all the states would together agree with the Commonwealth in the pooling of health functions and dollars across Australia. I believe that the best way forward would be to establish a joint Commonwealth-State Health Commission in any State where the Commonwealth and a particular State could agree, eg Tasmania, South Australia. The joint commission would have agreed coverage of Commonwealth and State programs with the pooling of funds for all those programs. Agreed governance would be essential. Local government could also be included. I have set out my proposal in what I have described ‘A coalition of the willing’ (www.newmatilda.com). It would be hoped that if the process could begin in one state, others would follow. Like almost every other issue in health, political leadership is the key. In my discussions with the ‘health industry’ there is widespread acceptance that there must be improved coordination of Commonwealth and State programs. The real obstacle is the lack of political leadership. That leadership is essential.
Holding Commonwealth and State elections on the same day would also be a useful way of coordinating Commonwealth and State policies within political parties.
Restructuring the health workforce
The restructuring of the ‘blue collar’ workforce has brought pain but also dramatic productivity improvements for the Australian economy and the community. But this restructuring has not touched the professions and certainly not the health sector where demarcations and restrictive practices abound. The health workforce is trained in separate boxes and works in separate boxes. The medical colleges for example, reinforce these separate boxes. Sectional interests are put ahead of the national interest, usually in the name of safety and quality. Fortunately the debate is changing and the recent report by the Productivity Commission is helpful to some degree in highlighting the problems and pointing the way forward.
The worst examples of restrictive practices that I know of are in the obstetrics field. In Australia less than 10% of normal births are managed by midwives. In the Netherlands it is over 70% and in the UK over 50%. There is great opportunity and need for restructuring — nurses undertaking greater responsibility for prescribing, diagnosis and triage in hospitals; nurse anaesthetists complementing and substituting for medically qualified anaesthetists; enrolled nurses taking on some of the tasks done by registered nurses; midwives substituting for obstetricians; practice nurses undertaking some of the work currently performed by GPs, including some prescribing, screening and triage. Why couldn’t we create a new broad-banded job of health practitioner which would include junior doctors, registrars and senior nurses in hospitals? The skills of pharmacists are under-utilised. Nurse practitioners have been skilled and qualified, but their numbers remain extremely low because of opposition by other professionals. Nurses hold the system together, but they are denied proper career opportunities both to their own detriment and the whole community.
I guestimate that workforce reform would achieve at least a productivity increase of 40% over 10 years and probably much more. The potential dividends are large as 70% of health costs are labour costs. Health workers comprise 7% of the Australian civilian workforce. The Productivity Commission estimate that a 10% efficiency improvement in health would deliver about $A8 b at the present time and $A16 b by 2050. I think the estimates are conservative. Health is a very labour intensive industry. We need up skilling, multi skilling, broad banding and teamwork — and quickly if we are to get better value for money.
We hear a lot about shortages of doctors and other clinicians. I am not always persuaded. Much of the shortage occurs in my view because of the rigid nature of health training and health work. There are plans to increase the number of doctors in Australia, but little effort is given to ways of changing the way in which doctors could be used more efficiently and health tasks more sensibly distributed. The last thing we want is to put money into workforce training for people to do the same jobs in the same way that they have done for the last century.
The virtues of the market are continually extolled. We should seriously consider auctioning provider numbers which in effect give the owner of the provider number a subsidised income. An auction would give doctors an opportunity to bid to practice in particular areas. Doctors are not short everywhere.
Health workforce reform requires political leadership. It is far more important than Work Choices for the future of Australia. The medical benefits scheme could also be a useful lever to force changes in work practices and open up opportunities for new and broad banded skills. Funding incentives to change are essential. Our Pharmaceutical Benefits Advisory Committee has shown how government buying power and incentives can be used for the benefit of the Australian community. Importantly, we need a health workforce that is built around patients’ needs and not provider demarcations.
A health model or a sickness model
We have a highly medicalised system based on treating sickness rather than keeping people healthy. Over 90% of Australian health dollars are spent on medical services for the sick, rather than on public health and prevention where spending is less than 2%. We spend our health dollars in arranging ambulances at the bottom of the cliff, rather than erecting handrails at the top.
The major health risks Australia faces require public health interventions rather than personal medical services.
§ Tobacco causes 20,000 deaths per annum and accounts for 10% of the total burden of disease. The total cost of tobacco smoking is over $20 b pa, about a quarter of our total health expenditure. The solution is not more medical services.
§ The nurturing and support of mothers and children in early childhood is increasingly obvious. Home visitation in the US for single disadvantaged, teenage mothers reveals that there is a $5 community saving for every $1 spent. Money spent in prevention produces better dividends than medical services.
§ Between 1985 and 1995 obesity among 7 to 15 year old Australians trebled. One in five Australian children are overweight or obese. We have a gathering storm which is going to cost us dearly both personally and nationally. Government intervention is essential to address the market failure which allows almost unfettered promotion of poor diet.
§ The major risk factor in poor health is poverty. Death rates in Australia vary dramatically depending on socio-economic circumstances. Poverty affects the health of people in many ways — poor nutrition, poor lifestyle, stress, poor nurturing, low self-esteem, exclusion and addiction. The main reason why aborigines have such poor health is because they are poor. Once again the solution is not more medical services.
The whole nature and the funding of public health requires urgent attention with higher priority for public health and quarantining it from medical services which are often seen to be more urgent but are usually less important.
Electronic health record program
The development of a national electronic health record system could be a key enabler, whereby individuals could voluntarily opt into the system and carry their own health records. It would reduce mistakes and improve safety. It would reduce the amount of testing when a patient goes to a new provider. It would improve the keeping of records and lessen the risk of wrong diagnosis and wrong prescription. It would lessen the costs of fragmentation and dysfunction between Commonwealth and State funded providers. The patient would carry the integrated and consolidated information across diagnostic boundaries. The aged and frail would particularly benefit from having their medical history easily and quickly available. There would be better integration between primary, secondary and tertiary health sectors.
The delivery of health services is a very labour and information intensive activity. The same is true in such industries as finance and banking. But whereas the banking sector spends about 10% of its operating budgets on IT, in health it is less than 2%. I have seen estimates ranging from 10% to 15% as the potential savings that could be achieved by efficient and effective implementation of health IT. That 10% would be about $9 b of Australia’s total health spending.
The business case is overwhelming. Unfortunately we are lagging behind other countries. The Commonwealth Government, together with the States, is developing ‘Health Connect’. There is concern that the project is not going well with the possibility that the project could be handed over to State jurisdictions. I would urge the Committee to examine this matter thoroughly.
Private health care, private insurance and personal responsibility for health care
The terms of reference highlight the importance of personal responsibility. I thoroughly agree, but in my view, the subsidy to private health insurance is a wasteful and inequitable way of achieving that result. I would like to suggest an alternative to ensure greater personal responsibility.
The subsidy to private health insurance ($3 b per annum) is not achieving its desired results. It is one of the most glaring examples of policy failure that I have seen.
§ The claim made that the subsidy has boosted private insurance numbers cannot be sustained. The improvements have been largely due to Lifetime Health Cover.
§ The subsidy is skewed to the wealthy. 80% of the richest 20% of Australians have private health insurance, whereas only about 25% of the poorest 20% of Australians have private health insurance. (See Governments Working Together, Victorian Department of Premier and Cabinet, 2004, p.80)
§ It has not taken pressure off public hospitals. It has opened up new private demand (Melbourne Institute of Applied Economics and Social Research Report to Victorian Department of Premier and Cabinet, 2004, p.39).
§ The private health insurance funds undermine the role of Medicare which seeks to contain costs through its buying power in the market. The funds are passive price takers and without managed care, as in the US, they underwrite rather than contain rising health costs. Their premiums are rising at about double the inflation rate.
§ The evidence is clear (see Agenda, Volume 12, No 2, 2005, pp.159 to 178, Ian McAuley) that encouraging private health insurance leads to escalating costs. The more a nation relies on private insurance to fund health care, the higher are its total health care costs, with the US being the most obvious case. If ever we wanted a warning about private health insurance we should look no further than the US.
It is important that we all accept greater responsibility for our own health decisions and outcomes. We must address the moral hazard problem. But that should be done, and it can be done, without detracting from a universal health system that delivers services to all. That delivery system will include both public and private systems and services.
Taking more responsibility for our health care costs can best be done through co-payments by individuals and the direct funding of private hospitals and not through subsidising inefficient and passive private health insurers. Why should private health insurance be propped up by corporate welfare when funds could be much better delivered directly to private hospitals?
Private hospitals perform an essential role in our health system. They should be funded directly either by means of a bed subsidy payment or using the same formula that is used in public hospitals to distribute hospital funds. It is based on Diagnostic Related Groups (DRGs). Had the funding of the $2.3 b in 2003/4 been directed wholly to private hospitals without passing through private insurance as a financial intermediary, they could have received an extra $1.2 b on top of their $1.1 b. Why waste so much public money in corporate welfare to private insurance funds when the money could be paid directly to the private hospitals.
Co-payments are the best way to ensure greater personal responsibility for health decisions. We have co-payments in respect of medical services, hospital services and pharmaceuticals. There are major inconsistencies between these co-payments. The most glaring is in bulk payments where there is no co-payment at all.
Since Medicare was introduced in 1975, incomes have increased substantially. For example, real annual disposable income per capita has increased from $24,000 in 1985 to $36,000 in 2006, an increase of 50%. Many well-off Australians could afford to pay more from their own pocket for access to a universal health system. That is the better way to do it, rather than providing corporate welfare to the health insurance industry. Making private health insurance a still more attractive option is the last thing we need in health.
It is clear that there are many areas in which we could achieve better value returns for our health dollars. Progress depends overwhelmingly on political leadership.
This is a submission made by the Centre for Policy Development chair John Menadue to the House of Representatives Standing Committee on Health and Ageing Enquiry into Health Funding — Sydney Friday 21 July 2006