Recently, the media reported that the Federal Government intends to reform the regulation of complementary medicines. In particular, Parliamentary Secretary Jan McLucas wants to improve complaint procedures and provide consumers with more reliable information.
Complementary medicines are now a big business with over $2 billion of sales annually. Up to two-thirds of the Australian adult population use at least one product annually. Consumers currently spend as much of their own money on these products as they do on conventional medicines. Despite this widespread use, the public is largely unaware that the regulation of these products is much weaker than that of conventional medicines. The end result is that it is impossible for consumers to know which complementary medicines offer genuine health benefits and which are merely snake oil. In addition, important safety issues, such as drug interactions, can be ignored.
Most complementary medicines are currently regulated as ‘listed’ products by the Therapeutic Goods Administration (TGA). The listing system provides rapid market entry at minimal cost. Product efficacy is not evaluated. The only routine checks made are that the ingredients are on TGA’s ‘relatively low-risk’ list and production is in accord with ‘Good Manufacturing Practice’. Sponsors are meant to certify that they hold evidence supporting the claims made about their product but their product information and promotional material is rarely reviewed.
By contrast, conventional medicines (‘registered’ products) are thoroughly evaluated by the TGA for safety, quality and efficacy before they are allowed onto the market. In addition, generic copies of clinically proven products must demonstrate therapeutic equivalence. Sponsors of both innovator and generic products must negotiate approved product information with the TGA and also provide consistent consumer medicines information and promotion. Not surprisingly, registration fees are substantial and the time taken can be protracted.
 This difference in regulatory rigour was originally justified on the grounds that complementary medicines were low-risk and less frequently used. Earlier this year, my colleagues and I published a paper on the outcome of this policy in the Medical Journal of Australia. We documented a proliferation of shonky products whose promotional claims could not be substantiated. Recent examples include Blackmores’ ‘Weight Loss Accelerate’ which claimed ‘three times greater weight-loss results than diet and exercise alone’; Symbion Consumer who claimed that ‘glucosamine could reduce the risk of osteoarthritis progression by 54 per cent’ and Arkopharma who claimed that ‘there are no reports in the literature of an interaction between glucosamine and warfarin’. None of these statements were in accord with the scientific literature and the last one also contradicts warnings by the Australian Adverse Drug Reaction Advisory Committee.
This difference in regulatory rigour was originally justified on the grounds that complementary medicines were low-risk and less frequently used. Earlier this year, my colleagues and I published a paper on the outcome of this policy in the Medical Journal of Australia. We documented a proliferation of shonky products whose promotional claims could not be substantiated. Recent examples include Blackmores’ ‘Weight Loss Accelerate’ which claimed ‘three times greater weight-loss results than diet and exercise alone’; Symbion Consumer who claimed that ‘glucosamine could reduce the risk of osteoarthritis progression by 54 per cent’ and Arkopharma who claimed that ‘there are no reports in the literature of an interaction between glucosamine and warfarin’. None of these statements were in accord with the scientific literature and the last one also contradicts warnings by the Australian Adverse Drug Reaction Advisory Committee.
Currently, the only way to correct such inaccuracies is by submitting complaints. However, the Complaint Resolution Panel is under-resourced, overloaded and lacks effective sanctions. It even lacks resources to follow-up its own determinations ⎯ which makes them easily ignored. It takes multiple complaints before non-compliance by a sponsor is passed to the TGA. That organisation, citing ‘commercial-in-confidence’ considerations, tells complainants nothing and publicises nothing. Clearly, complaint systems need to be better resourced and empowered with more effective sanctions. In addition, the TGA should be more transparent.
Analysis of successful complaints show they cluster around product categories such as weight loss, memory enhancement and arthritis relief. In 2007, the TGA was asked to review the efficacy of all ingredients used in weight loss products in the hope that up-stream evaluation would reduce the need for down-stream complaints. Industry concern watered down the scope of this review and the report has yet to see the light of day. The TGA (100 per cent funded by industry) has also failed to eliminate misleading weight loss product and pack names such as ‘Fat Blaster’, ‘Fat Blaster Max’, ‘FatMagnet’, ‘Slim Me’, ‘Weight Loss Accelerate’ and ‘Xantrax (High Potency Weight LossFormula)’.
The Government said it is waiting for a report from the National Prescribing Service (NPS) before considering specific reforms. The NPS was asked to research information needs of consumers and health professionals with respect to complementary medicines. The result seems self-evident; all medicines need objective and up-to-date information about their benefits and risks. Even if the risks of complementary medicine are relatively low, they can still harm consumers by adverse effects (e.g. rare cases of liver failure associated with Black Cohosh), drug interactions (e.g. bleeding associated with glucosamine and warfarin), wasting money and delaying access to more evidence-based therapy.
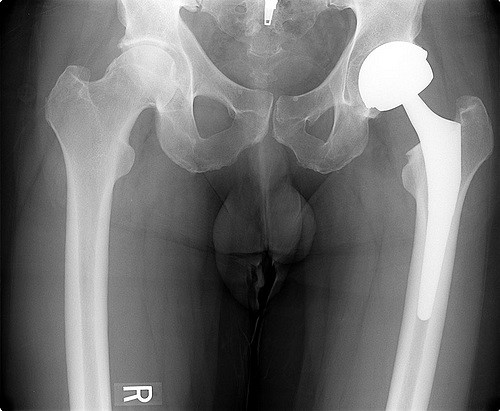
However, providing objective information about Australian complementary medicines is difficult because of the failure of the TGA to properly evaluate these products. Different complementary medicines containing the same ingredients are not necessarily chemically or therapeutically equivalent. Just as all red wine is not Grange Hermitage neither are all Australian glucosamine preparations (for example) necessarily equivalent to the few found clinically effective overseas.The industry cites patient experience as proof of efficacy but it is notoriously unreliable to judge the efficacy of a medicine from individual case reports, both because of the placebo response and also the natural remissions and exacerbations in chronic diseases such as osteoarthritis. Evaluation of properly conducted clinical trials is required. Another problem is that the current system has flooded the market with thousands of shonky products. It would be a Herculean task to clean up this Aegean stable.
Correspondence in the Medical Journal of Australia has proposed a pragmatic solution. Sponsors could choose to submit their product for independent evaluation by paying an additional fee. Products shown to be efficacious for specific indications by well conducted clinical trials (or proven therapeutic equivalence), with agreed objective information and ethical promotion would be awarded a Trade Mark of approval similar to the National Heart Foundation ‘Red Tick’. This measure, in addition to others suggested, would assist consumers chose efficacious products and support an evidence-based industry.
The challenge for the Federal Government is to overcome industry self-interest, and the perception of regulatory “capture”, and institute the necessary reforms.