Australians have some of the best health outcomes in the world, with high life expectancy and low death rates (although this is not the case for Indigenous Australians).
But despite these good outcomes, we have a ‘health system’ which is always under pressure and is groaning for relief. The system performs well only because of the very dedicated and professional people who uphold it.
I would like to highlight two big-picture issues at the heart of the problems in our health system. I believe that there is a growing community and government understanding of these two issues.
The first important issue is that we have a highly medicalised and specialised system based on treating sickness rather than keeping people well. One example of this medicalisation is that childbirth is treated as a sickness rather than a natural life event.
The major improvements in health outcomes over the centuries have not been in medicine but in prevention, early detection of chronic diseases and public health e.g. clean water, sanitation and vaccinations. But we spend minimal money in these areas. About 95% of our health dollar in Australia is spent on medical services. As a result, there are major health risks that are not being adequately addressed.
They are:
– Tobacco-related illnesses . Tobacco causes over 20,000 deaths in Australia per annum. Over 3 million Australians still smoke on a daily basis. Smoking accounts for 10% of the total burden of disease. Over 150,000 hospital separations per year are attributable to tobacco. The total national cost of tobacco smoking is over $20 b per annum, about a quarter total health expenditures. It is the biggest avoidable health risk in Australia. The solution is not more medical services.
– Neglect of early childhood development . The early years, even in utero, are critical for the future health of the individual. They are also important for the wider community. There are large individual and social dividends to be obtained by investing in early childhood. As Professor Graham Vimpani has pointed out in the Centre for Policy Development (link), regularly home visits in the United States, for example to single, disadvantaged, teenage mothers, results in savings of $5 for every $1 invested. Only South Australia seems to be getting the message. South Australia is to be congratulated on what it is doing in this field, particularly home visits to support mothers, babies and families in need. There is a long way to go, but South Australia is a pace setter for the rest of Australia. Underweight babies and neglected children are warning signs for the future. The risks in this area must be addressed in improved nurturing rather than in more medical services.
– Obesity . Another high-risk health problem for Australia, obesity is caused by excessive and bad diet, and a decline in exercise. It brings with it Type 2 diabetes, coronary heart disease, respiratory and other health problems. Obesity in Australian adults (25-67) has trebled from 6% in 1980 to over 18% in 2000. Between 1985 and 1995, obesity among 7 to 15 year old Australians tripled. One in 5 Australian children are over overweight or obese. Almost a quarter of Australian children and adolescents are overweight. It is a health time bomb loudly ticking. Again, the solution is not more medical services.
– Poverty . Poverty is the major risk factor in poor health, and the biggest cause of death. In South Australia for example, 38% more people die between the ages of 15 to 64 in Enfield than is expected given the death rate for the whole state. In the more affluent suburb of East Torrens, the death rate is 42% below the state average for 15 to 64 year olds. Poverty affects the health of people in many ways — poor nutrition, poor lifestyle, stress, poor nurturing, exclusion and addiction. The main reason why Indigenous Australians have poor health is because they are poor. Here again — the solution is not more medical services.
The effective response to these critical health risks — tobacco, neglect in early childhood, lifestyle, obesity and poverty — are not to be found primarily within the medical field. They are to be found in public health programs, e.g. educating people about lifestyle, exercise and diet; and wellness centres. Addressing these high health risks also means looking beyond the health field itself. The key to improved Indigenous Australian health involves self-esteem, training, jobs and housing — going far beyond both medical services and health.
 |
|
Thanks to Fiona Katauskas |
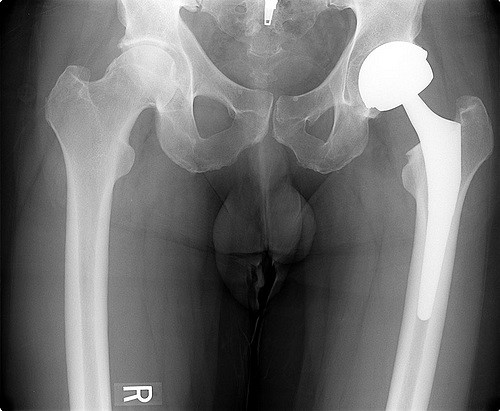
The second big picture issue is that we have a highly institutionalised health system. By institutionalised, I mean a highly hospital-centric system. Hospitals are our first resort. They should be our last resort. In the community we have the mindset that health equals hospitals. The public debate is invariably driven by issues concerning hospital beds and waiting lists. That is not where either the debate or the resources should be focused. I estimate that over 40% of people need not be in hospital if there was appropriate care outside in the community and, where possible, in the home. That is more consistent with personal autonomy and personal dignity. It is also better and cheaper for all concerned. The primary focus of care and good health must be in the community, not in hospitals. In my experience of informed community attitudes, the community has a very good sense of what is important. It is invariably mental health, indigenous health, women and children subject to violence, and health care as far as possible in the community and in the home.
We need a seismic shift away from medicalisation and institutionalisation in health. Public attention is focused on the medical and hospital, rather than on the important. We are focused on the urgent and short-term, rather than the important and long-term issues. The major solutions to our health risks are not to be found in the medical and hospital fields.
Unless we seriously address these two major flaws in our health system, it will remain continually under pressure. I do see signs of change in a better understanding of the two issues raised above. Recent meetings of the Prime Minister and the Premiers show the new trend. I first conducted a health inquiry in NSW in 2000 and in SA in 2003, and I am more optimistic now than then. But there are strong vested interests who would like to keep us medicalised and institutionalised when our priorities and resources should be elsewhere.